It's only natural to wonder or worry about how much weight you'll gain during your pregnancy. Although there's no exact answer as everyone's different, we look into the averages, plus the importance of sensible and healthy weight gain over the next nine months.
This page contains affiliate links, which means we may earn a small amount of money if a reader clicks through and makes a purchase. All our articles and reviews are written independently by the Netmums editorial team.
By now, we all know that 'eating for two' is just a myth, and that eating healthily and sensibly is important during pregnancy.
However healthy and active you are in pregnancy, weight gain is inevitable – you're growing and carrying a person inside you, after all!
How much weight should I gain during pregnacy?
The NHS doesn't give specific recommendations for how much weight you should aim to gain. However, they do say:
FREE NEWBORN NAPPIES
'Most pregnant women gain between 10kg and 12.5kg (22lb to 26lb), putting on most of the weight after week 20.'
That's about 1.5-2 stone.
Of course, every mum-to-be is different. Some will sport nothing more than a bump whereas others may say they look (and feel) like a beached whale by the time they reach their due date – it just depends.
The American Pregnancy Association gives different recommendations depending on your pre-pregnancy body mass index (BMI). They say you should aim to gain:
- 25-35 pounds if you were a healthy weight before pregnancy, with a BMI of 18.5-24.9
- 28-40 pounds if you were underweight before pregnancy with a BMI of less than 18.5
- 15-25 pounds if you were overweight before pregnancy with a BMI of 25-29.9
- 11-20 pounds if you were obese before pregnancy with a BMI of over 30
In the UK, healthcare officials recognise that everyone's different, so they don't give this advice. But you may find it helpful as a general guide.
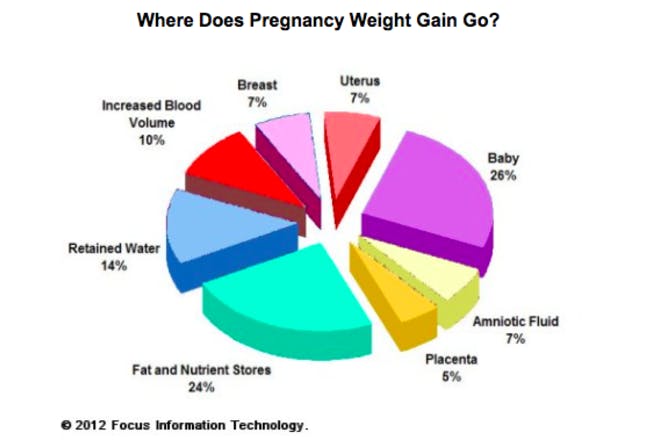
What causes weight gain in pregnancy?
The obvious answer is, of course, your growing baby.
As it grows, your waistline disappears and your bump expands – and you wouldn't want it any other way.
However, as well as pure baby weight, some women gain a lot of fluid, not to mention increased blood volume to support your growing baby.
But what else causes weight gain?
According to the NHS, 'much of the extra weight is due to your baby growing, but your body will also be storing fat, ready to make breast milk after your baby is born.'
And don't forget the placenta, too. Reports suggest it weighs roughly one sixth of what your baby does at birth. So if the average baby weighs around 3.3kg, a placenta will weigh around 0.7kg. That's pretty weighty!
Should you eat more during pregnancy?
Experts suggest that you don't need to change your diet significantly in the first six months of pregnancy.
Instead you should stick to the guideline calorific intake for women of 1,800-2,000 calories per day – easier said than done if your cravings for chocolate or ice cream kick in!
Just try eating as healthily as you can and staying as active as you can.
Other than that, avoid 'eating for two'.
Official guidelines recommend that mums-to-be only need an extra 200 calories in your last trimester, as studies have found that a significant number of expectant mothers who eat more than they need to run the risk of being overweight decades later.
If you were wondering, 200 calories is the equivalent of a small sandwich, a piece of toast or a glass of orange juice – not a tub of ice cream, sadly.
Weight gain in pregnancy: what are the risks?
If you're overweight or obese at the time you fall pregnant, you're at greater risk of experiencing problems in pregnancy, such as:
- miscarriage
- gestational diabetes
- high blood pressure
- pre-eclampsia
- blood clots
- foetal abnormalities
- complex birth
- heavier bleeding after birth
- increased birth weight
If you have a BMI above 35, NHS guidelines state that you should be cared for in a consultant-led hospital or antenatal unit. Which means if you want a home birth, you will be advised against it.
Monitoring your weight during pregnancy
You'll be weighed at your initial ‘booking in’ antenatal appointment.
Generally speaking, your GP or midwife might suggest a weight management plan for you if you weigh:
- more than 100kg (15.5 stone)
- less than 50kg (8 stone)
They may also go by your BMI (Body Mass Index) - this tool is used to measure weight in relation to height and is generally accepted as the most useful way to establish whether a person's weight is healthy for their build.
The medical profession use the following guidelines for all individuals, not just pregnant women:
- Those with a BMI below 18.5 are considered underweight
- Those with a BMI between 18.5 and 24.9 are considered normal weight
- Those with a BMI between 25.0 and 29.9 are considered overweight
- Those with a BMI of 30.0 and above are considered obese
If your weight and BMI is considered normal, you won't necessarily be weighed again unless your midwife has concerns, i.e if you have been very overweight or underweight during the pregnancy.
You may also need to be weighed towards the end of your pregnancy, if you're expected to have a caesarean section. This is done to help the anaesthetist calculate the volume of drugs you may need.
What to do if you're overweight and pregnant?
If you're overweight, focus on not gaining too much extra weight during pregnancy and eat sensibly, as opposed to dieting.
Stay active throughout your pregnancy (e.g. walking, swimming) – this will help you manage your weight and also help prepare your body for labour.
Dieting during pregnancy
If you were following a diet before you conceived, it's worth talking to your midwife about what it consists of before carrying on with it through your pregnancy.
If it cuts out food groups or involves fasting, it won't be a good idea to carry on as your baby needs a whole range of nutrients and regular meals to grow and develop. You'll also need your energy!
However, some healthy eating and wellness plans, such as Slimming World are doable when required during pregnancy.
Find out more about Slimming World when you're pregnant here.
WW (formerly Weight Watchers) isn't allowed during pregnancy.
‘When members get pregnant, we suspend their membership until after they’ve had their baby,' says Zoe Griffiths, public health manager at WW.
Being underweight in pregnancy: what are the risks?
Problems in pregnancy and birth aren't just associated with being overweight. If you're underweight you may encounter issues, too.
Women who have always been slim may struggle to adapt to their new body shape, and may restrict their diet in an attempt to keep the pregnancy pounds at bay.
But dieting or remaining significantly underweight once you get pregnant could reduce the baby’s birth weight and put them at risk.
If you're not getting all the vital nutrients which a healthy, balanced diet provides, the baby will be missing out on important nutrients, too, causing problems for their development.
Gaining too little weight during pregnancy can also increase the chance of:
• premature birth
• having a baby with a low birth weight.
What to do if you're underweight and pregnant?
If you struggle to put on weight during pregnancy, try to increase your calorie intake. Make simple swaps like opting for full-fat milk instead of semi-skimmed, and choosing foods like bananas and avocado that combine extra calories with extra nutrients for you and your baby.
Try eating regularly too, 'grazing' on fruit, veg and seeds during the day.
Slow down on your regular exercises and if it's your busy work schedule that is stopping you from eating right, then try to take regular breaks to eat.
Morning sickness and weight loss
For some women, weight loss is a side effect of severe morning sickness . In most cases, morning sickness eases as you approach the second trimester and it doesn't usually pose any risk to the baby.
However, if you are concerned about any symptoms associated with nausea and sickness – for example, if the sickness is very severe and you are losing weight – it's important to ask your midwife for advice.
If you're extremely sick and unable to keep anything down, you may have a condition called Hyperemesis Gravidarum (HG).
Women suffering from HG may lose more than 10% of their pre-pregnancy weight and could become dehydrated, so it's vital to consult a medical professional if you're worried.
How to get help managing your weight during pregnancy
Most GPs and midwives should be able to offer you sufficient support and advice, but if you feel you need extra help, you should ask to be referred to a dietitian.
They will be able to draw up a healthy eating plan, which is safe to follow in pregnancy, and will help you avoid any excessive weight gain (or help you gin weight if you're currently underweight).
It’s important to remember that medical guidelines are quite clear that pregnancy is not a time to embark on a restrictive diet. Always check with your midwife before starting any new eating plan.
What to Expect When You're Expecting by Heidi Murkoff is a must-read book for all expectant parents. See more details here at Amazon.
You can also buy it here at Waterstones.
Why not chat to other mums-to-be about how they manage their weight during pregnancy in our chat thread below?
Related stories
Your complete A-Z of pregnancy food and drink safety